Grow Your Knowledge about Health Plan Options
Open Enrollment is now closed. If you have questions about your benefits or would like to make changes to your benefits due to a qualified life event, please contact the HR Solution Center at AskHR@virginia.edu.
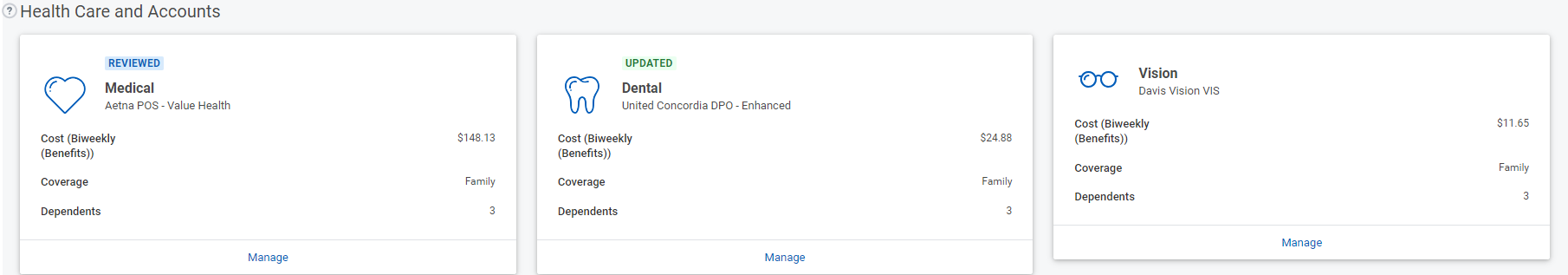
Open Enrollment is a time for all UVA benefits-eligible employees and team members to learn about, carefully review, and elect benefits for the following plan year starting January 1, 2024. These benefits include health and dental plans, vision coverage, Health Savings Account, Flexible Spending Account, and Dependent Daycare Reimbursement Account.
Unless you experience a qualified life event like having a baby or getting married, making changes to these benefits can only be done during Open Enrollment, which this year runs October 2 through 13, 2023.
To make the Open Enrollment experience as beneficial for you as possible, you have both in-person and virtual opportunities to learn what you need to know to pre-plan your future emotional, physical, and financial well-being. Whether you want to meet in person or virtually, UVA HR is here to help.
Key Takeaways
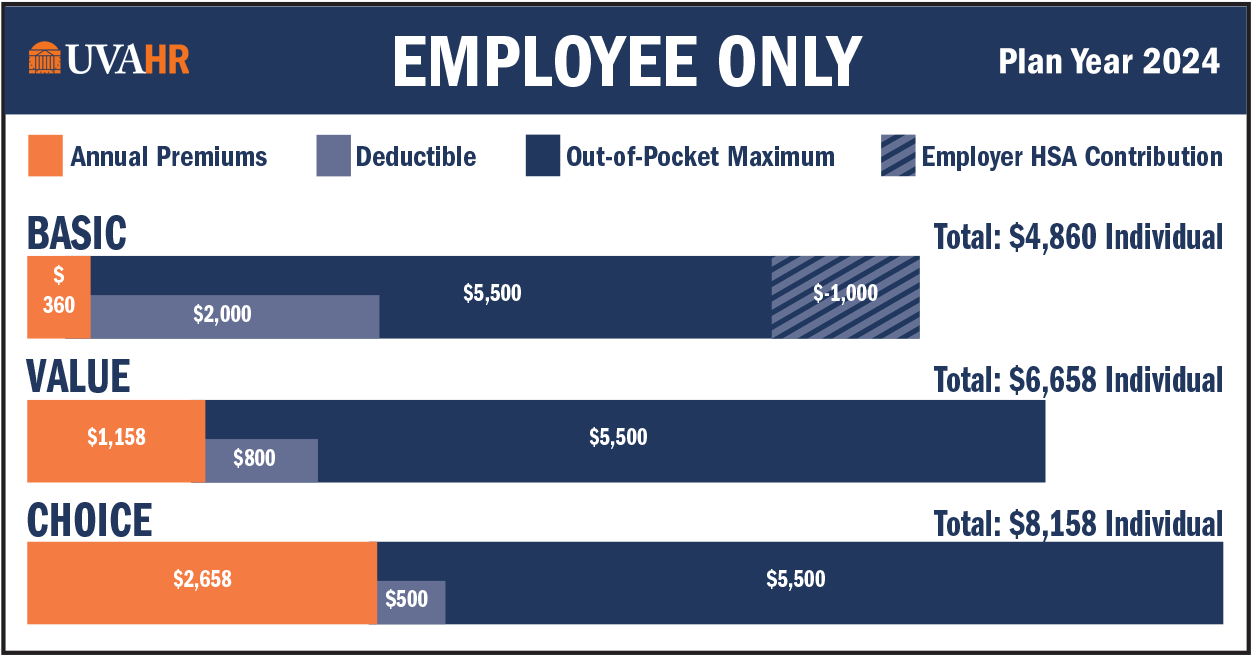
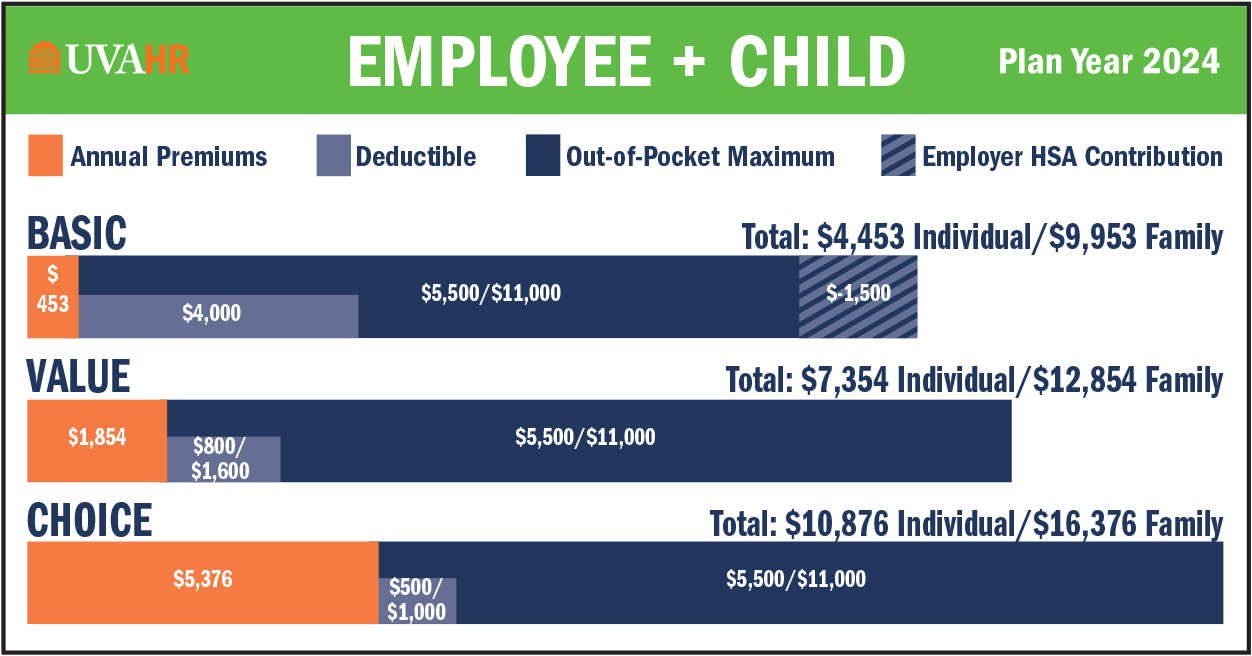
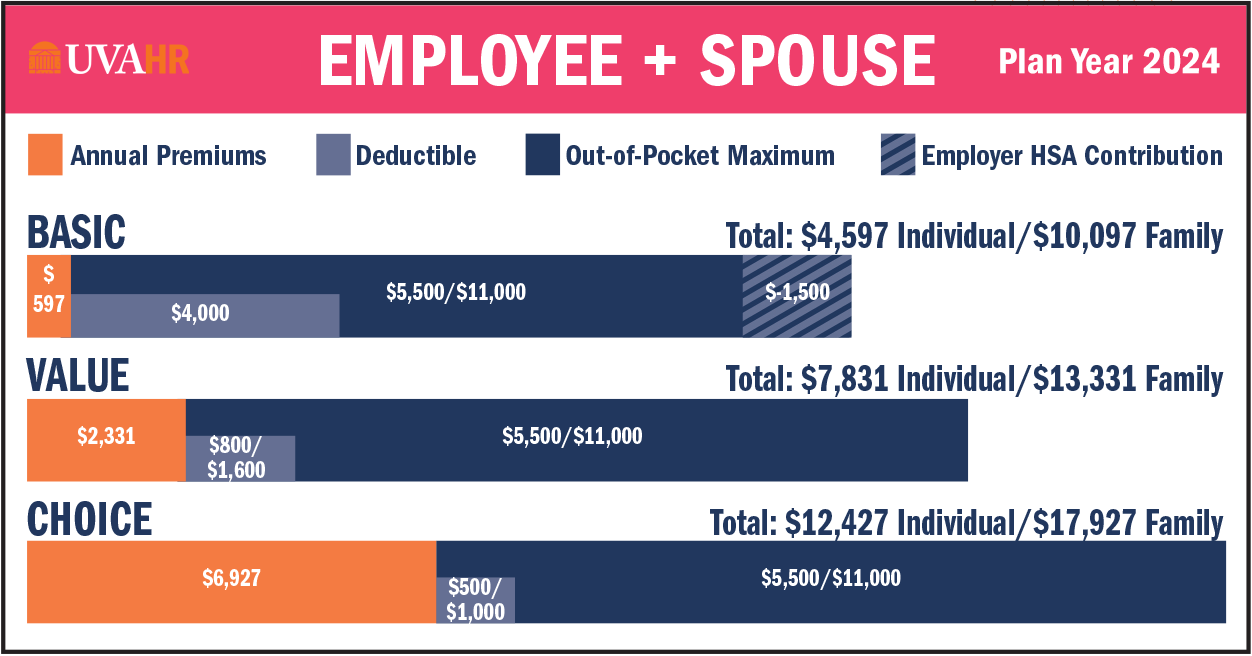
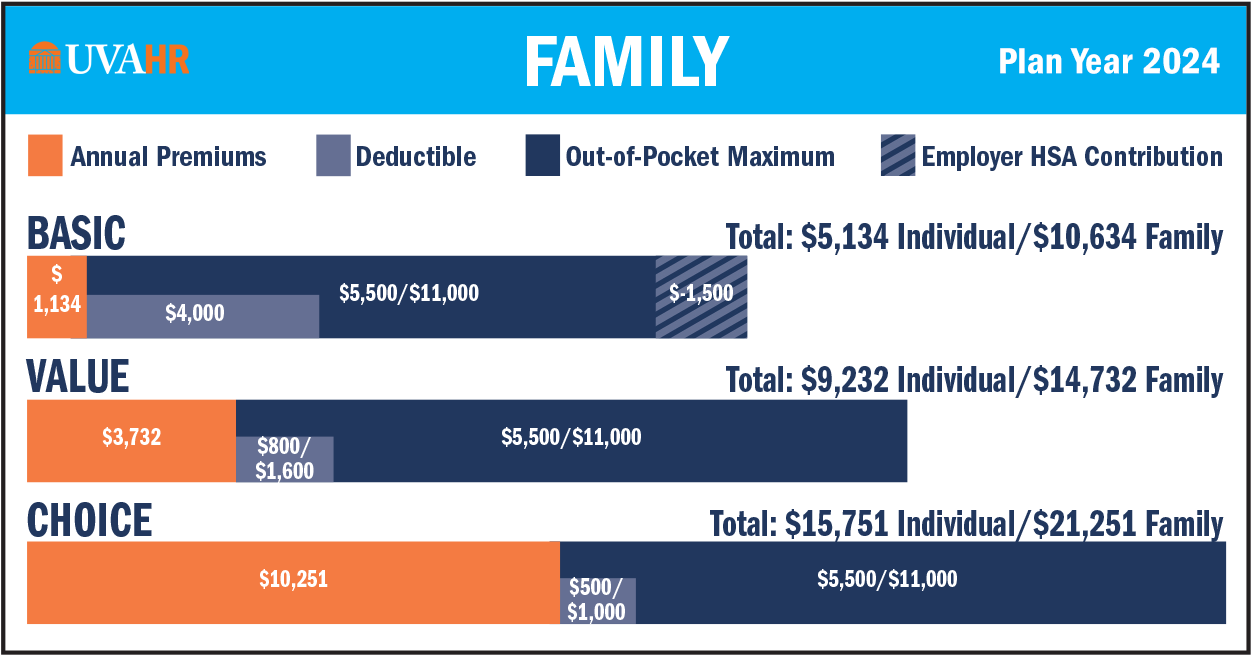
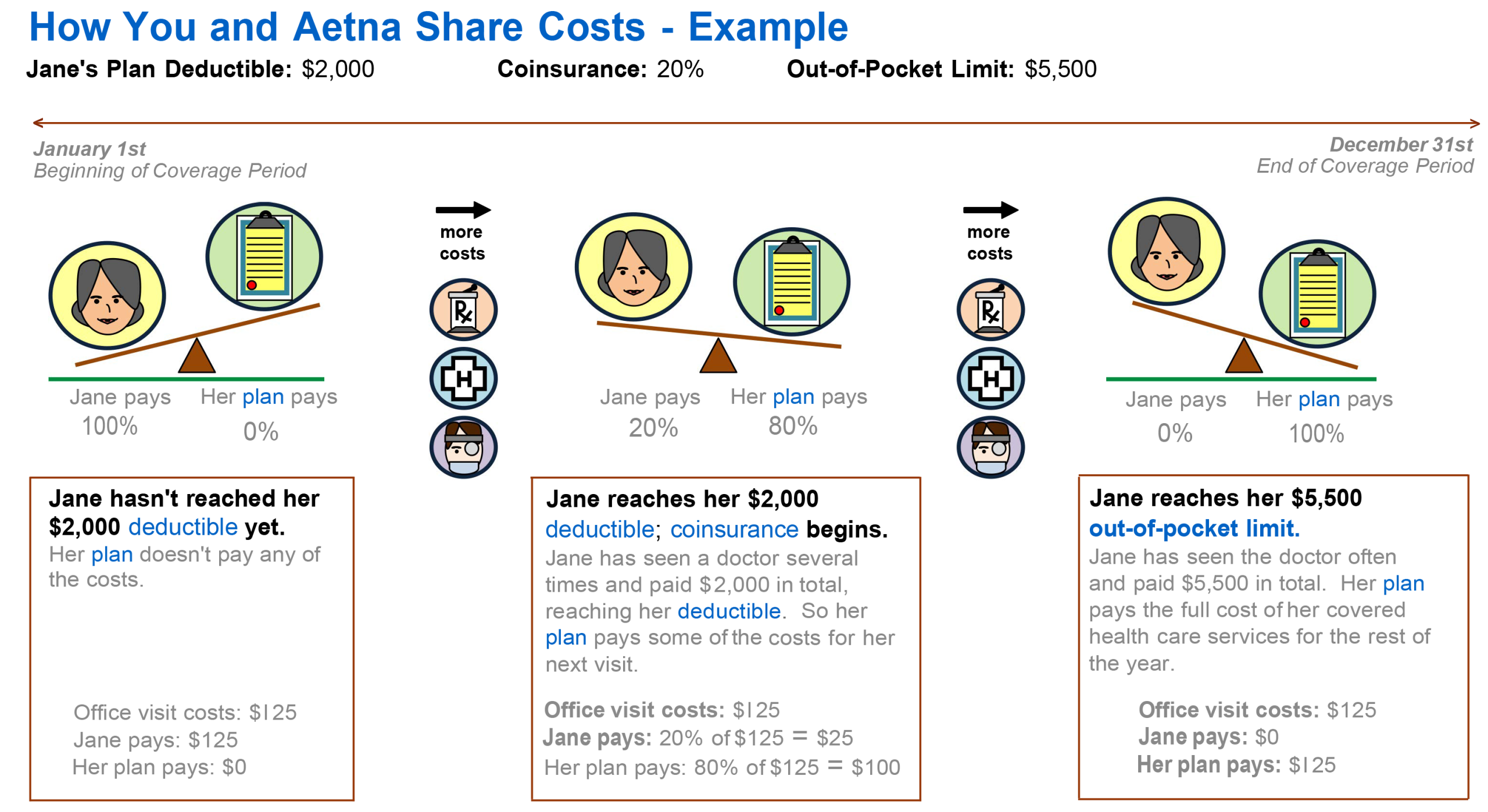
Health Plan Premiums - UVA Health Plan rates will increase to account for the rising costs in medical and prescription claims. As a self-insured health plan, the Plan is paid for by employee and employer contributions, and rising prices and employee utilization have an impact on the cost of the health plan. While employee premium rates will increase in 2024, the employer contribution will cover the greatest part of the increases.
- There are no changes to deductibles, copays, or coverage
- There are no changes to the Aetna vision discount program
- There are no changes to the Prescription Drug program
HSA Employee Contribution - The employee maximum contribution to the Health Savings Account for Basic Health participants will increase in 2024 (employee maximum contribution limits include employer seed funds, which will remain the same):
- Individual - $4,150 (from $3,850 in 2023)
- Family - $8,300 (from $7,750 in 2023)
- Catch-up (age 55+) - $1,000 (no change)
Summary of Material Modifications - Open Enrollment materials constitute a Summary of Material Modifications for UVA Health Plan changes effective Jan. 1, 2024.